Become invisible and walk into a Chiropractic, Physiotherapy or Massage Therapy office one day. Watch them speak with a patient who has back pain or maybe a little bit of knee pain. You may hear the following:
-you need stability exercises
-these muscles are very tight
-you need therapy as you don’t want this degeneration to progress
-no more running or arthritis will certainly flare up and you will have real problems down the road
-you have dysfunctional movement patterns
-your glut muscles don’t turn on
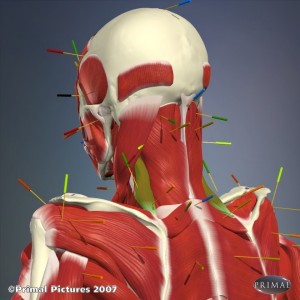
-oh, it hurts here (pressing on upper traps). There some adhesions in the muscle
-I need to see you 2-3 times a week for the next 4-6 weeks.
All of the above statements are from good, well meaning people. And some of these statements might even be appropriate under certain conditions. These statements typically are not from the quacks and crooks that look to exploit anyone who has been in a car accident or might have fallen off their bike when they were six (and therefore their spine is permanently in trouble because of this “trauma’).
My concern is how all of these things sound to our patients - which is different from what we hear. If you tell someone they need stability exercises they probable assume their spine is unstable. That probably does not sound good to a patient with an incredible amount of pain. When we poke on areas that are “tight” or “sore” in everyone (e.g. the upper traps, you can’t find someone who is not tender there) we catastrophize, comment on how tight it is and reinforce a pain belief with our poking and create beliefs in people that there is something wrong with their muscles.
Not encouraging patients to resume their normal activities and to keep active contributes to fear and movement avoidance.
Telling patients that the way they move is dysfunctional based on an arbitrary standard of how someone should move again creates the belief in people that something is seriously wrong when there is usually no serious dysfunction.
Seeing someone 3x/week for 6 weeks for whiplash or a simple backache. Come on. Common sense says this is bad practice even though it is somehow in many guidelines.
The bottom line is we need to watch our words. I am no exception, I catch myself doing this too often. An unstable spine means something completely different to a therapist than it does to a patient. The phrase degenerative joint disease should be banned - they have a joint that is changing like everyone’s joints and most minor symptoms have nothing to do with those normal changes.
Just some thoughts,
Greg Lehman